

Theory
Depression involves changes at many levels of a person, biological, psychological, social and existential. This article only discusses the biological.
The dominant theory is called the Catecholamine theory, or sometimes the Monoamine theory.
Essentially it is that one or more of the monoamine neurotransmitters, serotonin (a.k.a. 5-HT), noradrenaline (a.k.a. norepinephrine), or dopamine, become, for one reason or another, less able to carry nerve signals across nerve junctions, called synapses. It is generally assumed, but remains unproven, that the problem is due to a shortage of the neurotransmiitter.
1) Shortage of neurotransmitter.
 |
|
2) Increase in 5-HT2 receptors.
Serotonin (5-HT) travels across the synapse and connects with one of about 17 different 5-HT receptors. Some people, possibly especially those who are anxious or have been traumatised, appear to increase the number of 5-HT2a, 5-HT2c and 5-HT3 receptors. If SSRI or SNRI antidepressants are started abruptly, these receptors may be flooded, with side effects including insomnia and sexual problems (5-HT2a), agitation (5-HT2c), nausea (5-HT3), and possibly an increase in suicidality. Some studies suggest that 'dysfunctional attitudes' are related to 5-HT2 receptors 10.
Certain antidepressants including mirtazapine, mianserin, and nefazodone block the 5-HT2a receptor, as do antipsychotics such as olanzapine, quetiapine, and risperidone. They may therefore be useful as augmenting agents during early treatment with SSRIs or SNRIs.
A metaphorical story illustrates the issues.
The Synapse Restaurant.
Imagine you own a restaurant, with 17 tables, each representing one type of serotonin receptor. When things are going well, the restaurant is full, there is a happy hubbub of conversation and laughter, especially from Table One (5-HT1). Your waiters scurry around, tips are plentiful and the cash register keeps ringing.But when a depression occurs, few customers come to your restaurant. Money is tight. Not many people sit on Table One, so the mood and ambience drops. Potential customers look in the door, note that the restaurant doesn't seem very popular, and go somewhere else. In addition, the number of chairs on Table Two (5-HT2) is increased. Table Two is associated with insomnia, agitation, and sexual problems.
When we give an SSRI or SNRI, the strategy is equivalent to locking the door OUT of the restaurant. Serotonin Reuptake Inhibition. Potential customers can come in to check out the menu, but they can't get out. They have to stay. The good news is that several of them sit on Table One, so mood lifts. The bad news is that even more (because of the extra chairs) sit on Table Two, leading to a range of side-effects.
The implications of the metaphor are:
- Start SSRIs or SNRIs very slowly. Don't slam the door shut abruptly. Give it time, and some of the extra chairs on Table Two will get removed.
- Put a reserved sign on Table Two. Use an augmenting drug with 5-HT2 blocking qualities such as mirtazapine (Avanza), mianserin (Tolvon), or olanzapine (Zyprexa).
What follows is a selection of some of the excellent illustrations from 'Essential Psychopharmacology' by Stephen M. Stahl. 11

Normal synapse, no depression.

Depression caused by neurotransmitter deficiency
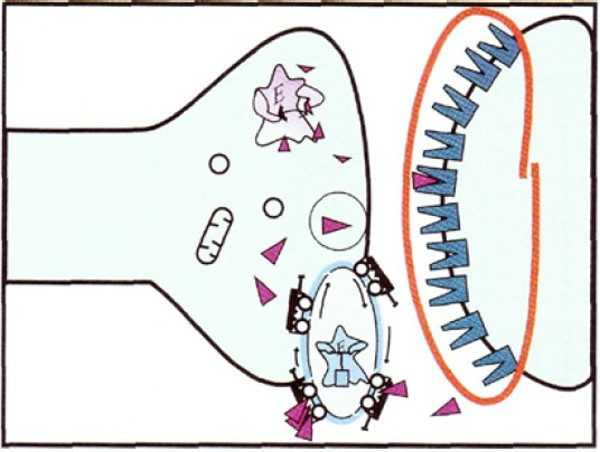
As a result of the depletion of neurotransmitters, the receptors increase ('upregulate')

Reuptake blocking antidepressant (TCA, SSRI or SNRI) causes increase in neurotransmitters to normal state
SSRI blocks the reuptake pump, causing more neurotransmitter to be in the synapse. If the SSRI dose is introduced too quickly, there may be over-stimulation of some of those receptors that cause side-effects (eg 5-HT2a, 5-HT2c and 5-HT3 receptors. This can cause insomnia and sexual problems (5-HT2a), agitation (5-HT2c), nausea (5-HT3), and possibly an increase in suicidality.

Increase in neurotransmitter causes receptors to down-regulate, eventually.

There are several different types of post-synaptic 5-HT receptors.
Mechanism of action of serotonin selective reuptake inhibitors (SSRIs)—part 1. Depicted here is a serotonin neuron in a depressed patient. In depression, the serotonin neuron is conceptualized as having a relative deficiency of the neurotransmitter serotonin. Also, the number of serotonin receptors is up-regulated, or increased, including presynaptic autoreceptors as well as postsynaptic receptors.

Mechanism of action of serotonin selective reuptake inhibitors (SSRIs)—part 2. When an SSRI is administered, it immediately blocks the serotonin reuptake pump (see icon of an SSRI drug capsule blocking the reuptake pump). However, this causes serotonin to increase initially only in the somatodendritic area of the serotonin neuron (left) and not in the axon terminals (right).

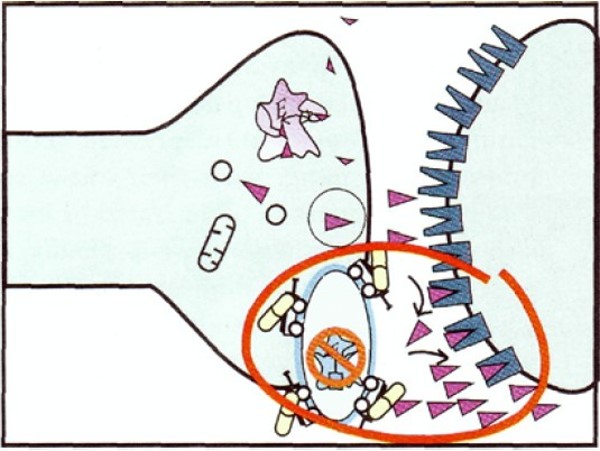
Mechanism of action of serotonin selective reuptake inhibitors (SSRIs)—part
3. The consequence of serotonin increasing in the somatodendritic area of the
serotonin neuron, as depicted above, is to cause the somatodendritic serotonin
1A autoreceptors to desensitize or down-regulate (red circle).

Mechanism of action of serotonin selective reuptake inhibitors (SSRIs)—part 4. Once the somatodendritic autoreceptors down-regulate as depicted in Figure 6-37, there is no longer inhibition of impulse flow in the serotonin neuron. Thus, neuronal impulse flow is turned on. The consequence of this is release of serotonin in the axon terminal (red circle). However, this increase is delayed as compared with the increase of serotonin in the somatodendritic areas of the serotonin neuron, depicted above. This delay is the result of the time it takes for somatodendritic serotonin to down-regulate the serotonin 1A autoreceptors and turn on neuronal impulse flow in the serotonin neuron. This delay may explain why antidepressants do not relieve depression immediately. It is also the reason why the mechanism of action of antidepressants may be linked to increasing neuronal impulse flow in serotonin neurons, with serotonin levels increasing at axon terminals before an SSRI can exert its antidepressant effects.
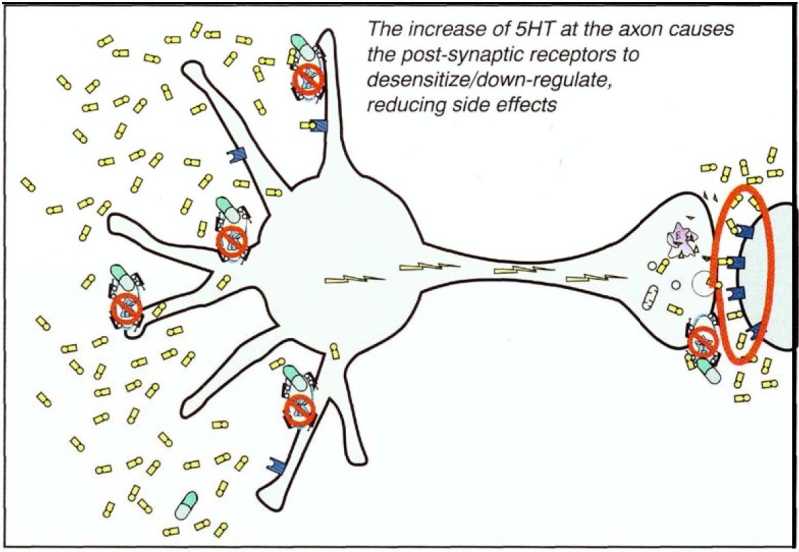
Mechanism of action of serotonin selective reuptake inhibitors (SSRIs)—part 5. Finally, once the SSRIs have blocked the reuptake pump, increased somatodendritic serotonin, desensitized somatodendritic serotonin 1A autoreceptors, turned on neuronal impulse flow, and increased release of serotonin from axon terminals, the final step shown here may be the desensitization of postsynaptic serotonin receptors. This desensitization may mediate the reduction of side effects of SSRIs as tolerance develops.

Mirtazapine actions at serotonin (5HT) synapses. When presynaptic alpha 2 heteroreceptors are blocked, 5HT is released, but it is directed to the 5HT1A receptor because 5HT actions at 5HT2A, 5HT2C, and 5HT3 receptors are blocked. The result is that antidepressant and anxiolytic actions are preserved but the side effects associated with stimulating 5HT2A, 5HT2C, and 5HT3 receptors are blocked. However, sedation and weight gain may result from these actions.
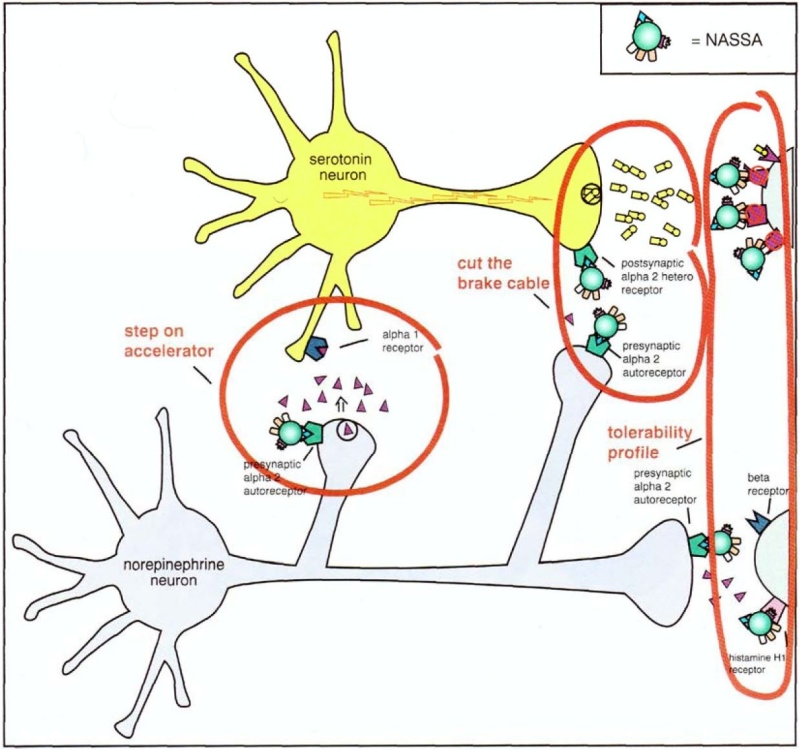
An overview of the actions of mirtazapine. This includes the actions of alpha 2 antagonists, that is, the therapeutic actions of cutting the NE brake cable while stepping on the 5HT accelerator (left circle), as well as cutting the 5HT brake cable (middle circle). This increases both 5HT and NE neurotransmission. On the right are the additional actions of mirtazapine beyond alpha 2 antagonism. These postsynaptic actions mainly account for the tolerability profile of mirtazapine.